male Partner Examination
- Evaluation of male partner also plays a significant role in evaluation of infertility.
- Male partner contributes to about 30% as a sole reason for infertility and another 20% as combined factor.
- More often than not infertility specialists ignore this part, and the only evaluation done for the male partner is a semen analysis.
Male partner evaluation is done in a very systematic manner at Sunflower Infertility & IVF Center
- History
- Examination
- Blood Test
- Karyotyping
- Sperm DFI
- Scrotal Doppler
- Oral Medicine
- Surgical Treatment (TESA, PESA, Micro TESA)
A detailed history includes age of male partner, married life duration, addictions like smoking, alcohol consumption, frequency of intercourse, history of coital dysfunction if any ( erectile or ejaculatory dysfunction), history of any major medical surgical illness ( like diabetes mellitus, hypertension, inguinal hernia, hydrocele, surgery for undescended testes), any significant family history

Physical examination
- Height, weight, BMI of male partner is noted as obesity also is known to impact fertility. His vital signs ( temperature, pulse rate, B.P.) examination is performed and if necessary a detailed systemic examination is done.
- Genital examination is done to determine size of testes, presence of varicocele, epididymal cysts or any other pathologies.
sunflower success numbers
1500+
IVF and ICSI procedures a year.
21000+
Live births by IVF and ICSI technology.
Life member
AOGS, AICOG, FOGSI, ISAR, ESHRE, ASRM, IFFS, IMA.
Success rate
70% to 76% in IVF ART.
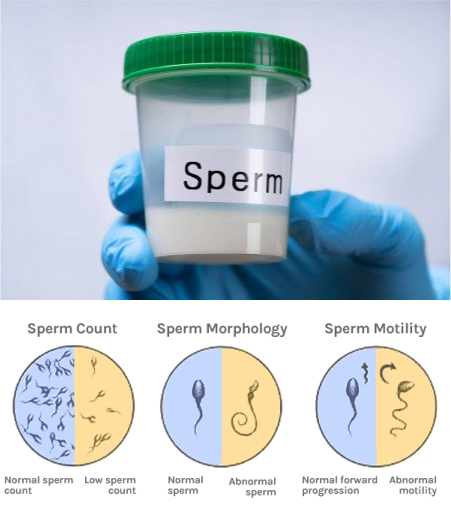
Semen analysis and blood tests
Most centres do only a semen analysis of the male partner and if it is normal don’t do any further investigations for the male partner. But this is where we beg to differ, as a few blood investigations are important even for the male partner, like complete blood count to rule out any anemia , random blood sugar ( to screen for diabetes) Hb electrophoresis, Serum FSH and a total testosterone level may help uncover certain trends even though semen analysis is normal, viral diseases like Hepatitis B and HIV which can have parent to child transmission.
About 25% of all infertility is caused by a sperm defect and 40-50% of infertility cases have a sperm defect as the main cause, or a contributing cause.
Method for Collection :- Masturbation, Coitus interruptus, special condom
[No spermatocidal agents ]
Abstinence Period :- 3-4 days
Collection area :- In close proximity to the laboratory (to avoid long transport)
Container :- Big mouth polypropelene plastic jar
Sonography of the Scrotum
Ultrasonography (US) with a high-frequency (7.5-10-MHz) transducer has become the imaging modality of choice for examination of the scrotum. US examination can provide information valuable for the differential diagnosis of a variety of disease processes involving the scrotum that have similar clinical manifestations (eg, pain, swelling, or presence of mass). The pathologic condition that may be at the origin of such symptoms can vary from testicular torsion to infection to malignancy. The ability of color and power Doppler US to demonstrate testicular perfusion aids in reaching a specific diagnosis in patients with acute scrotal pain. This review covers the anatomy of the scrotum and the scanning protocol for scrotal US, as well as detailed descriptions of disease processes and their US appearances. Newly described conditions such as intratesticular varicoceles and other benign intratesticular cystic lesions are also discussed.
Ultrasonography (US) performed with a high-frequency transducer and the use of pulsed and color Doppler modes is the imaging modality of choice for evaluating acute and nonacute scrotal disease. Many of these disease processes, including testicular torsion, epididymo-orchitis, and intratesticular tumor, produce the common symptom of pain at presentation, and differentiation of these conditions and disorders is important for determining the appropriate treatment. US with a high-frequency transducer helps to better characterize intrascrotal lesions, and in many instances the findings suggest more specific diagnoses. High-frequency US in its present state can help identify certain benign intratesticular lesions, resulting in testes-sparing surgery. Familiarity with US characteristics and the examination pitfalls of scrotal US is essential for establishing the correct diagnosis and initiating treatment.
This review is organized on an organ basis and proceeds from superficial to deep structures. We review the anatomy of the scrotum and its contents, US scanning techniques, and US features of various pathologic conditions. This review is intended to bring the reader up to date with new technology and to provide insights into the US diagnosis of scrotal disorders. Newly described entities, such as intratesticular varicocele and other benign intratesticular cystic lesions, are discussed in detail.
Scrotal doppler sonography when indicated
- In case of low sperm count and motility, a scrotal sonography may uncover certain pathologies which may be missed on physical examination.
- A scrotal sonography helps in determining testicular size, position especially in cases of undescended testis, presence or absence of vas, epididymal cyst, spermatocele, presence of varicose veins and grading
- Small testicular size is suggestive of testicular failure
- Absent vas deferens with dilated epididymal head and normal size testicular failure is a classical finding in cases of azoospermia with congenital bilateral absent vas deferens.
The genetic material of the sperm is tightly packaged into a small nucleus in the head of the sperm, this basically assists in giving the sperm a form which can help it to swim, but this tight packaging /also puts the sperm at risk of DNA damage.